MaxorPlus
MaxorPlus has over 29 years of experience and an award winning customer service team that will be available for 24/7/365 support.
A new Drug Search tool is available to SmartHealth members. This tool will allow members to search medications to determine the formulary tier, drug class coverage, and if a prior authorization is required.
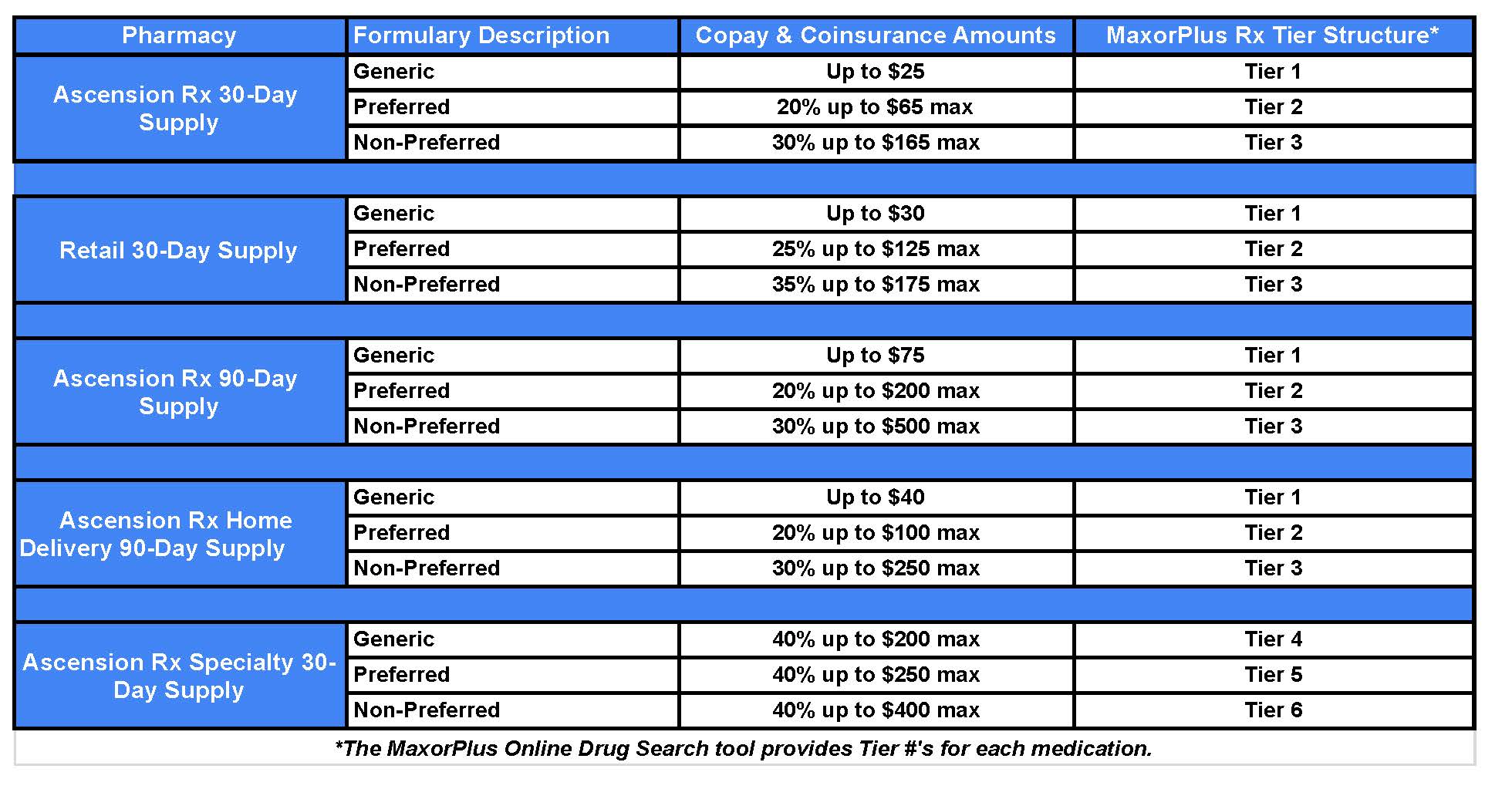
Pharmacy out-of-pocket costs for 2025
Pharmacy Benefit Details
Important pharmacy benefit and ID card information
A new pharmacy ID card will be sent to you for MaxorPlus's drug plan in the beginning of the year. Please note that this card is different from your medical card. To fill prescriptions, you must use your new prescription ID card.
If you need a new card, please call 888-492-6811 or download the Ascension One app to access a digital copy of your card.
Important pharmacy documents
-
Maintenance medicationsMaintenance medications are medications taken at home on a consistent schedule to treat chronic or long-term conditions. This may include oral, injectable, inhaled, ophthalmic and topical medications. Specialty medications are not considered maintenance medications within your pharmacy benefit. These two classifications have different definitions and requirements within SmartHealth. Learn more about maintenance medications including types of medications and where to fill here.
-
Glossary of terms
-
Ascension Rx pharmacies
-
SmartHealth Specialty Prescription Drugs
SmartHealth specialty prescription drugs are Tier 4, 5 and 6 on this online drug search tool
A specialty medication is considered a high-cost drug used to treat complex conditions. These drugs are available from your pharmacy benefits, and are usually self-administered. Specialty medications are prescription drugs that are filled by a specialty pharmacy because they have requirements that can only be fulfilled within our Exclusive Specialty Pharmacy Network. Specialty medications meet or exceed a cost of $830 for a 30 days supply, require special handling, require additional patient education, and/or require clinical pharmacy intervention to ensure safe use of the specialty drug.
Specialty medications must be filled within our Exclusive Ascension Specialty Pharmacy network. Some medications may be subject to participation in the Flexible Copay program.*Information on the Flexible Copay program appears below on this website. -
Manual claim forms
This claim form can be used to request reimbursement of covered expenses paid out of pocket.
-
Continuous glucose monitors
Continuous glucose monitors (CGM) are important tools for tracking and managing diabetes. Your plan offers coverage for two CGM sensors under your pharmacy benefit: the Dexcom and Abbott FreeStyle Libre.
-
Diabetic benefit
Ascension preferred diabetic medications and supplies receive a reduced copay when filled at an ARx pharmacy.
Medications: Novolog (additional may be added)
Supplies: T1 (preferred generic) & T2 (preferred brand)
Continuous Glucose Monitors: T2 (preferred brand)
-
2025 SmartHealth ACA ($0) Medication List
2025 SmartHealth ACA ($0) Medication List
Medications available at no cost to members under Patient Protection and Affordable Care Act (PPACA).
-
2025 SmartHealth HDHP Preventative Medication List
2025 preventative medication drug list
Preventive medications are used to help avoid disease and maintain health. For those members on a high deductible health plan (HDHP), before the deductible has been met, these medications will only be subject to copay/coinsurance and still apply towards out-of-pocket max. If your medication is not a maintenance medication on this list, continue to fill it at your local pharmacy.
SmartHealth Flexible Copay Program
Every year, the cost for some specialty medications might change and go up, which means you could pay more out of pocket. To help with this, Smart Health will continue offering the SmartHealth Flexible Copay program. This program works with drug manufacturers' copay assistance programs to help lower your out-of-pocket costs for these expensive medications.
However, manufacturer assistance programs may change or end at any time during the year. If that happens, you'll need to pay the regular copay for your prescription based on your SmartHealth plan. Keep in mind that this assistance is provided by the drug manufacturer, not by Ascension Rx or SmartHealth.
If you have a high copay and would like to find out if you are eligible, call the SmartHealth Flexible Copay program at 833-980-2352 and select option 7 to get started.
Provider administered specialty medications or infusion therapies
(Your provider or physician's office must submit the prior authorization)
All physician-administered specialty medications or infusion therapies are subject to precertification notification or prior authorization (PA) approval. For a product list with current requirements, please see the medical benefit drug list.
Have questions?
- Call 833-980-2352 to speak to a member of the Ascension Rx prior authorization team.
- Call 888-492-6811 to confirm a patient's SmartHealth plan eligibility.
To submit a precertification notification or prior authorization request for a physician-administered product or infusion therapy:
- Download the form: Medical benefit drug precertification notification and PA form
- Complete and sign the form
- Submit the completed and signed form:
- Via fax to 512-831-5499
- Via the Jiva Provider Portal at https://bit.ly/AscensionProviderPortal